You don’t think about your health until you have to. One moment you’re moving through life effortlessly, and the next, a sudden fever, injury, or diagnosis forces everything to stop. In that moment, nothing matters more than access to care, to relief, to survival. On the individual level, health is the foundation of everything, and yet it’s often invisible until it begins to fail. The same is true for nations. A healthy population is the backbone of a strong economy, a stable society, and a resilient future. But like personal health, national healthcare is too often overlooked until crisis hits. Pakistan stands at precisely that juncture, where the absence of a robust, accessible healthcare system has moved from a long-standing issue to a national emergency.
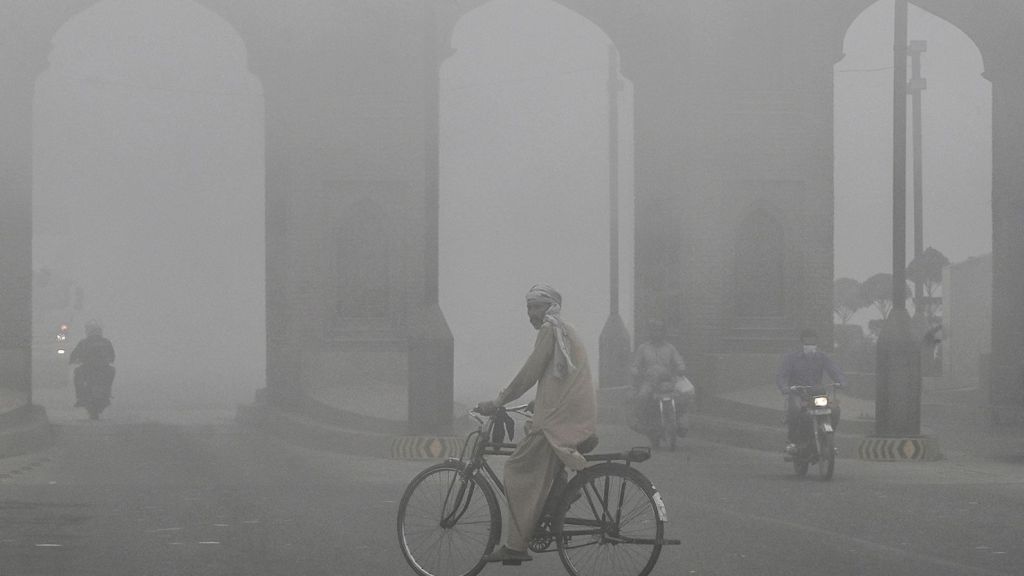
Beyond emergency care, tens of millions of Pakistanis face a growing burden of chronic disease that erodes both individual well-being and national productivity. Non-communicable diseases such as diabetes, cardiovascular disorders, and respiratory illnesses account for over 58% of all deaths in Pakistan, according to WHO estimates. A major contributing factor to this crisis is the country’s deteriorating environmental health. Pakistan is consistently ranked among the top five most polluted countries in the world, with Lahore frequently recording PM2.5 levels exceeding 200 µg/m³ — more than 10 times the WHO’s safe threshold. In 2023, over 11 million children in Punjab alone were exposed to toxic smog conditions, with 40,000 seeking treatment for respiratory complications during a single high-smog period. Chronic exposure to this air pollution is linked to increasing rates of asthma, lung disease, heart attacks, and stroke. Meanwhile, the economic cost is staggering: pollution-related illnesses reduce labor productivity and burden an already overstretched healthcare system. As the environment becomes more hostile to human health, the country faces a health crisis not rooted in contagion, but in the air people breathe every day.
Lack of Existing Facilities
Pakistan’s healthcare infrastructure is severely underdeveloped relative to the size and needs of its population. With over 229 million people, the country has just 1,276 hospitals and approximately 146,000 hospital beds. This equates to 0.5 beds per 1,000 people, significantly below the global average of 3.3. In many districts, particularly in rural areas, a single hospital may serve hundreds of thousands of people, often without specialized care or sufficient equipment.
Emergency services are fragmented and inconsistent. Pakistan lacks a centralized ambulance network and a standardized emergency dispatch system. Many ambulances operate without trained medical personnel, essential life-support equipment, or GPS connectivity. In urgent situations, patients are frequently transported in private vehicles without medical supervision. These delays contribute to higher mortality and morbidity, particularly for trauma, stroke, and cardiac cases that depend on rapid response.
Hospitals often operate beyond capacity. Intensive care units and emergency departments are overcrowded. Diagnostic services, including CT and MRI, are limited to a small number of urban centers and are frequently unavailable due to equipment failure or maintenance issues. Operating rooms face long backlogs, and access to specialists is highly uneven across regions.
Moreover, there is no unified national health information system. Most facilities rely on paper-based records, leading to inefficiencies in treatment, poor continuity of care, and challenges in data collection for public health planning. Access to care is further limited by geographic disparities and cost barriers, with many rural populations having no nearby facilities and urban centers being financially inaccessible to lower-income groups.
These infrastructure deficiencies affect every level of care delivery and reflect a systemic lack of investment and coordination. Without significant intervention, they will continue to limit Pakistan’s ability to respond to both routine and large-scale health challenges.
Staffing Shortages
In addition to infrastructure deficiencies, Pakistan faces a critical shortage of trained healthcare professionals. As of 2022, there were approximately 274,135 registered doctors in the country, resulting in a doctor-to-patient ratio of roughly 1:1,300. This falls short of the World Health Organization’s recommended ratio of 1:1,000. The shortage is more pronounced in rural and underserved areas, where many facilities operate without full-time physicians or specialists.
The nursing workforce is similarly underdeveloped. With just over 121,000 nurses and 44,000 midwives, Pakistan’s nurse-to-patient ratio remains among the lowest in the region. This imbalance places additional strain on physicians and contributes to overburdened hospitals, delays in treatment, and diminished quality of care.
Training capacity also remains limited. Medical colleges and nursing schools produce a fraction of the professionals needed to meet current demand. Retention is another major challenge. A significant number of trained doctors and nurses leave the country each year for better opportunities abroad, resulting in a continued drain of skilled personnel from the domestic health system.
In the absence of sufficient staffing, existing facilities are unable to function effectively. Operating rooms, maternity wards, emergency departments, and intensive care units require multidisciplinary teams to run safely. Without adequate personnel, the expansion of physical infrastructure alone will not be enough to improve health outcomes.
Addressing the human resource gap is essential. Any national strategy aimed at strengthening healthcare delivery must include substantial investment in workforce training, retention, and equitable distribution across urban and rural areas.
Action Steps
- Build More Public Hospitals, Equitably Distributed
The most urgent priority is expanding hospital infrastructure. The government should commit to building at least 2,000 new public hospitals over the next 10 to 15 years, with a focus on underserved rural and peri-urban areas. Every district should have at least one general hospital with surgery, maternity, diagnostics, and emergency care. - Raise the National Bed Capacity
Pakistan currently has only 0.5 hospital beds per 1,000 people. The goal should be to reach at least 1.5 beds per 1,000 by 2035. This requires expanding existing facilities, especially in growing cities, and building new ones in areas where access is limited. - Develop a National Emergency Care Network
A nationwide emergency system with a unified helpline, trained ambulance services, and GPS-enabled dispatch centers should be rolled out across all provinces. Ambulances must be standardized with minimum equipment and staffed by trained EMTs. - Expand the Healthcare Workforce
Pakistan needs more doctors, nurses, and allied health professionals. Government-funded medical and nursing schools should increase intake by at least 50% over the next five years. Incentives such as housing, career growth, and rural service bonuses should be provided to professionals who serve in remote areas. - Build a Unified National Health Information System
Digitized patient records and real-time data systems should connect every hospital and clinic in the country. This ensures faster, safer care and enables better national planning and disease monitoring. The system must be public, secure, and interoperable. - Introduce Universal Health Coverage
Pakistan should strengthen and expand its public insurance systems, like the Sehat Sahulat Program, to cover the entire population. This model, similar to Taiwan’s, ensures that care is accessible to all, while providers are reimbursed fairly through a national health fund. - Support Local Production of Medical Equipment and Medicines
Investment should be directed toward domestic manufacturing of essential pharmaceuticals, diagnostic kits, medical devices, and hospital equipment. This will reduce import dependence, create jobs, and build national resilience during emergencies. - Strengthen and Standardize Primary Healthcare
Every union council should have a fully functional basic health unit (BHU) with regular staff, essential medicines, and simple diagnostic tools. Maternal and child health services, vaccination, and chronic disease screening should be delivered locally and reliably. - Promote Preventive and Environmental Health
Pollution, unsafe water, and poor nutrition contribute heavily to disease. National health strategy must address environmental factors as core public health issues. This includes air quality monitoring, urban smog control, sanitation infrastructure, and public health education. - Regulate, Integrate, and Collaborate with the Private Sector
The private sector plays a role, especially in urban areas. It should be integrated into national health planning through regulation, data reporting, and service contracts. Large private hospitals should participate in national coverage schemes to ensure standards and equity. - Create a National Health Authority for Planning and Oversight
A dedicated, transparent body should oversee infrastructure development, hospital accreditation, workforce planning, and emergency preparedness. This authority must publish annual performance reports and ensure accountability to the public. - Prepare for Public Health Emergencies
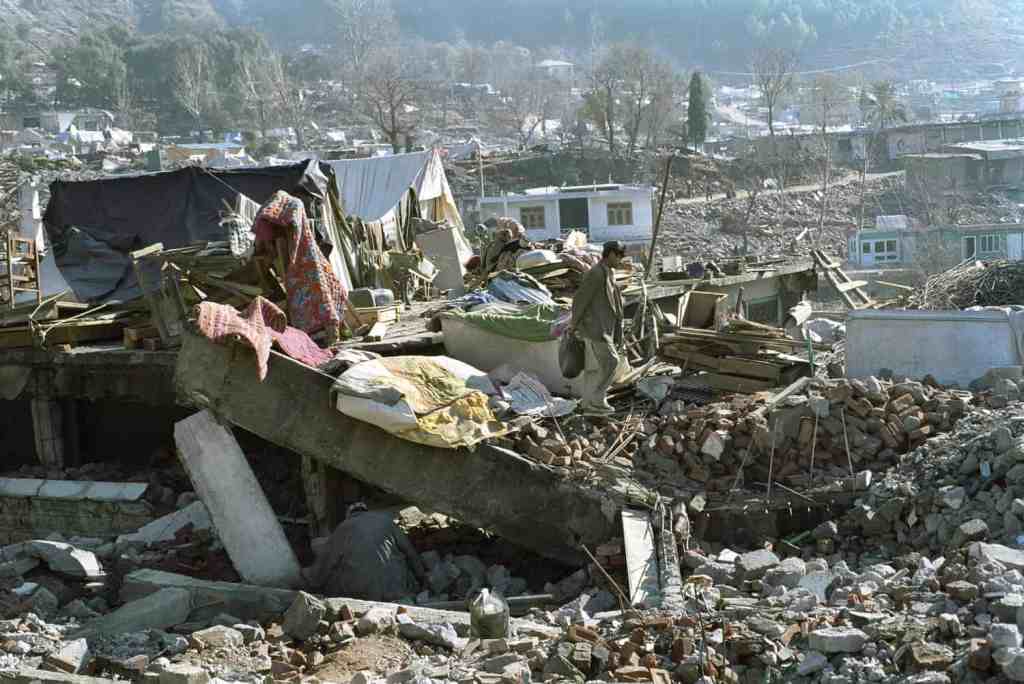
Pakistan should invest in mobile clinics, stockpiled medical reserves, and trained emergency response teams. Each province should have the ability to quickly scale up care in the event of a flood, earthquake, epidemic, or air quality crisis.
Healthcare is the foundation upon which a nation’s strength is built. For Pakistan, the time has come to move beyond patchwork fixes and commit to a comprehensive, nationally coordinated system that guarantees care for every citizen. This is not just a matter of policy, it is a matter of principle. A country cannot progress when its people are left behind in sickness. With the right planning, investment, and political will, Pakistan can build a healthcare system that is equitable, resilient, and rooted in the public good. The path forward is clear.